A team of researchers from the Florida State University College of Medicine has found that an amino acid produced by the brain could play a crucial role in preventing a type of epileptic seizure.
Temporal lobe epileptic seizures are debilitating and can cause lasting damage in patients, including neuronal death and loss of neuron function.
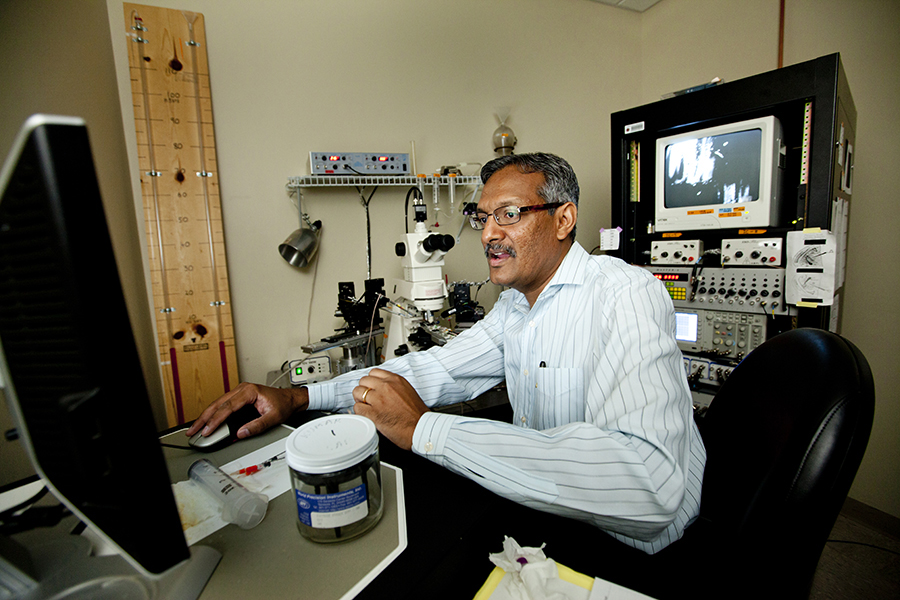
Sanjay Kumar, an associate professor in the College of Medicine’s Department of Biomedical Sciences, and his team are paving the way toward finding effective therapies for this disease.
The research team found a mechanism in the brain responsible for triggering epileptic seizures. Their research indicates that an amino acid known as D-serine could work with the mechanism to help prevent epileptic seizures, thereby also preventing the death of neural cells that accompanies them.
The team’s findings were published in the journal Nature Communications.
The temporal lobe processes sensory information and creates memories, comprehends language and controls emotions. Temporal lobe epilepsy (TLE) is the most common form of epilepsy in adults and is not improved with current anti-epileptic medications.
“A hallmark of TLE is the loss of a vulnerable population of neurons in a particular brain region called the entorhinal area,” Kumar said. “We’re trying to understand why neurons die in this brain region in the first place. From there, is there anything that we can do to stop these neurons from dying? It’s a very fundamental question.”
To help further understand TLE pathophysiology, the Kumar lab studies underlying receptors in the brain. Receptors are proteins located in the gaps, or junctions, between two or more communicating neurons. They convert signals between the neurons, aiding in their communication.
Kumar and his team discovered a new type of receptor that they informally named the “FSU receptor” in the entorhinal cortex of the brain. The FSU receptor is a potential target for TLE therapy.
“What’s striking about this receptor is that it is highly calcium-permeable, which is what we believe underlies the hyperexcitability and the damage to neurons in this region,” Kumar said.
When FSU receptors allow too much calcium to enter neurons, TLE patients experience epileptic seizures as neurons become overstimulated from the influx. The overstimulation, or hyperexcitability, is what causes neurons to die, a process known as excitotoxicity.
The research team also found that the amino acid D-serine blocks these receptors to prevent excess levels of calcium from reaching neurons, thereby preventing seizure activity and neuronal death.
“What’s unique about D-serine, unlike any other drugs that are out there, is that D-serine is made in the brain itself, so it’s well-tolerated by the brain,” Kumar said. “Many medications that deal with treating TLE are not well-tolerated, but given that this is made in the brain, it works very well.”
With assistance from Michael Roper’s lab in the FSU Department of Chemistry and Biochemistry, the research team found that D-serine levels were depleted in epileptic animals, indicating that TLE patients may not produce D-serine like they should.
“The loss of D-serine essentially removes the brakes on these neurons, making them hyperexcitable,” Kumar said. “Then, the calcium comes in and causes excitotoxicity, which is the reason why neurons die. So, if we provide the brakes — if we provide D-serine — then you don’t get that loss of neurons.”
Kumar’s research points to neuroinflammation as the cause for diminished D-serine levels in the entorhinal cortex of the brain. D-serine is typically produced by glial cells, but neuroinflammation experienced as part of TLE causes cellular and molecular changes in the brain that can prevent it from being produced.
The next step in exploring D-serine as a viable therapy is investigating potential administration techniques.
“We have to find creative ways to administer D-serine to that particular region of the human brain,” Kumar said. “Getting it to that right place is the challenge. We have to look at what effect it has when administered locally to that region of the brain compared to systemically through an IV, for example.”
TLE often results from an injury such as a concussion or other traumatic brain injury. When administered to the appropriate region, D-serine has been shown to work in preventing the secondary effects of such an injury.
“A pie-in-the-sky type idea is a hypothetical scenario where you were to have a nebulizer, or have people inhale D-serine, go play football, and if they experience a concussion, no neurons would be lost because the D-serine would provide a sort of cushion just in case there is a traumatic brain injury that can lead to loss of neurons in the temporal lobe,” Kumar said.
“There are some very interesting questions to ask and solve,” he added. “The important thing is that we’ve outlined the basic bread-and-butter mechanisms of why D-serine works. What we’ve established is the discovery of the receptors, discovery of the antagonist for these receptors (D-serine), how it works and how to prevent the emergence of TLE. The mechanisms and pathophysiology are as relevant to the animal model as they are to human beings, and that’s where the excitement lies.”
The research was funded in part by grants from the Council on Research and Creativity and College of Medicine at Florida State University, the Epilepsy Foundation and the National Institutes of Health.
FSU Department of Biomedical Sciences research faculty member Stephen Beesley, graduate student Thomas Sullenberger and undergraduate research assistants Kathryn Crotty, Roshan Ailani and Cameron D’Orio contributed to this study, as well as Kimberly Evans, Emmanuel Ogunkunle and Michael Roper in the FSU Department of Chemistry and Biochemistry.