
A Florida State University researcher joined an international team using brain scans and machine-learning algorithms to determine which areas of the brain were most associated with learning speech among deaf children with cochlear implants.
The breakthrough, published in the journal Proceedings of the National Academy of Sciences of the United States of America, puts the team on track to develop a tool that can help predict which children will need more intensive speech therapy.
“That’s where we want to go with this,” said Erin Ingvalson, assistant professor in FSU’s School of Communication Science and Disorders. “We want to develop a measure that clinicians can use to identify which children will need more speech-language support after they get their cochlear implant. That kind of tool would allow us to intervene with focused therapy that increases their ability to learn language.”
The cochlear implant can be a life-changing technology. However, over the past decade, researchers have documented a gap in speech outcomes among children who receive the device. Some acquire language and catch up to their peers with normal hearing, while others lag well behind.
“We want to figure out how to close that gap,” said Ingvalson, who began work on the project as a postdoctoral student at Northwestern University in Illinois.
The team of researchers used MRI scans of children at Lurie Children’s Hospital of Chicago to identify changes in the brain among those with hearing loss.
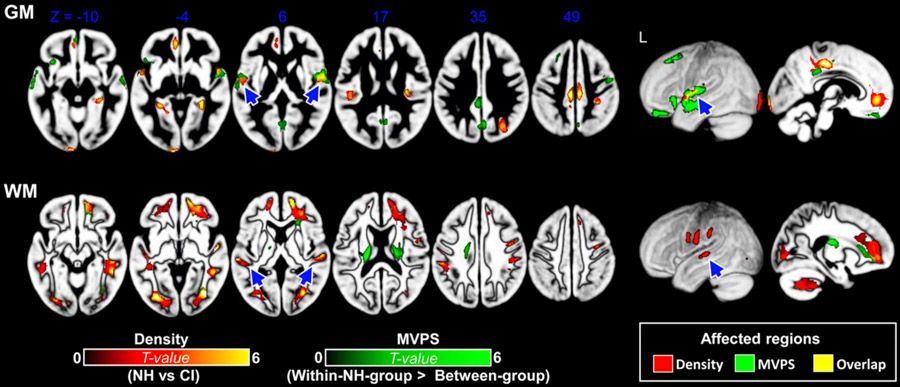
Using those scans and machine-learning algorithms, the team identified regions in the brain, including the fronto-parietal network, that would best predict a child’s ability to perceive and learn speech after receiving a cochlear implant.
The discovery opens the door to developing a clinically viable tool that uses a brain scan to determine which children will need more intensive speech-language support after they receive a cochlear implant.
“We want these children to be successful cochlear-implant users, so we no longer have this gap in speech outcomes among those with hearing loss,” Ingvalson said.
Decades of research show a cochlear implant is the most effective treatment for children born with significant hearing loss when hearing aids fail to help them develop age-appropriate listening and language. Helping them acquire language and literacy is critical for academic success, social and emotional well-being and getting a job.
Co-senior author Dr. Nancy M. Young — medical director of Audiology and Cochlear Implant Programs at Lurie Children’s Hospital and a surgeon and professor at Northwestern University Feinberg School of Medicine — said researchers have not had a reliable way to predict which children with hearing loss would have more difficulty learning language.
“Our study is the first to provide clinicians and caregivers with concrete information about how much language improvement can be expected given the child’s brain development before surgery,” Young said. “The ability to forecast children at risk is the critical first step to improving outcomes. It creates a foundation for development of customized therapies.”
Successful development of hearing and speech depends on both the ear and the brain. When auditory areas of the brain are not stimulated in children, they experience abnormal patterns of brain development.
“We used MRI to capture these abnormal patterns before cochlear implantation and constructed a machine-learning algorithm to predict language development with a relatively high degree of accuracy, specificity and sensitivity,” said co-senior author Professor Patrick C. M. Wong, director of the Brain and Mind Institute at The Chinese University of Hong Kong. “Although the current algorithm is built for children with hearing impairment, more research is underway to predict language development in other pediatric populations.”
The next step for the team is to expand the project to more hospitals and track children with cochlear implants over a longer period.
“It’s exciting to get to this stage of the project and rewarding to see some robust results,” Ingvalson said. “You can see the clinical relevance, and you know it will have a real impact on children’s quality of life. That gives extra significance to the work and becomes a strong motivator to keep going.”




